January's Case of the Month - 2026
Hyperaldosteronism- Is CKD your only differential?
PATIENT INFORMATION:
Age: 11 years
Gender: Male neutered
Species: Feline
Breed: Domestic Long Hair
Weight: 11.9 lbs
BCS 5/9
HISTORY:
First presented for second opinion 1/14/2025 for large SQ /dermal mass (12.7 x 11.4 x 8.9cm) on ventral abdomen, firmly attached to body wall. FNAs were inconclusive due to low cellularity. Mass was surgically removed 1/24/2025 with histopathologic diagnosis of Liposarcoma-- incompletely removed. Regrowth noted at both ends of surgical scar in early May 2025. Second surgery was performed 5/16/25 to remove regrowth, but the owner declined second histopathology due to finances. Chemotherapy recommended-- Doxorubicin injections q 3 weeks for 5 treatments (20-25mg/m2 IV). Recheck CBC and pretreatment with Diphenhydramine prior to each injection. Chemotherapy began June 2025 and continued q 3 weeks through September 2025. Marked weight loss of 7.7 lbs during this period of chemotherapy, and further weight loss of 3.7 lbs from September to AUS in November. (Beginning weight 23.3 lbs, 11.9 lbs prior to AUS). AUS ordered to assess for metastasis and to evaluate kidneys due to elevated kidney values, hypokalemia, hyporexia and weight loss. Cat had gradually developed a plantigrade stance/gait since last chemotherapy in September.
CLINICAL SIGNS:
hyporexia
weight loss of 3.7 lbs since 9/27/25
plantigrade stance
BIOCHEMICAL ABNORMALITIES:
Amylase (1912 IU/L) High
BUN 69 mg/dl High
CK 2400 IU/L High
Creat 4.7 mg/dl High
Na/K ratio 59 High
Potassium 2.5 mEq/L Low
Mg 2.3 mEq/L Low
SDMA 27.5 UG/dl High
T4 1.5 Normal
CBC Normal
ULTRASOUND FINDINGS:
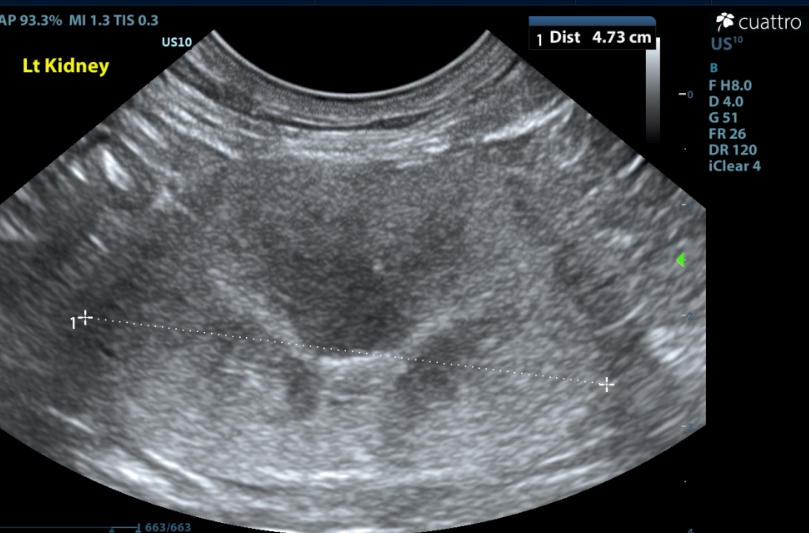
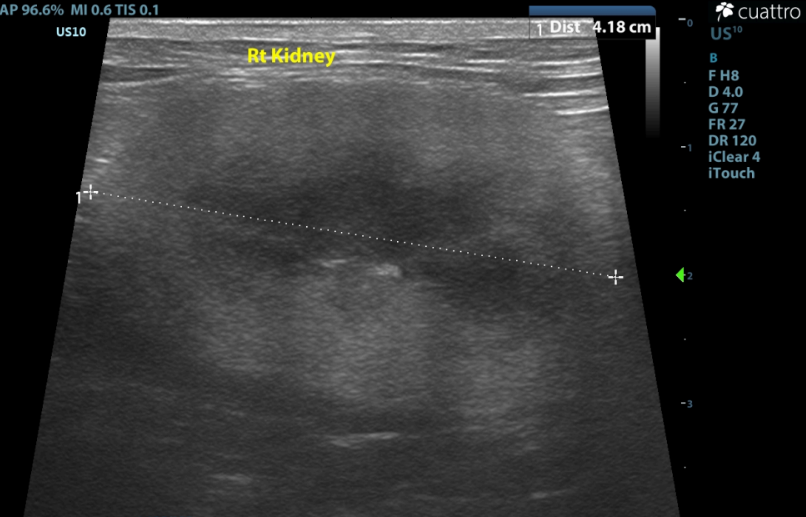
Kidneys ---Both kidneys have borderline to enlarged size (Lt/Rt =4.7 /4.1cm ) and normal shape with coarse moderately hyperechoic renal cortices which are disproportionately large. There is moderate loss of the corticomedullary junction distinction. No pyelectasia seen.
(normal renal size 3.2cm to 4.2cm; Renal Size in Cats, JAVMA, July 2005, Vo
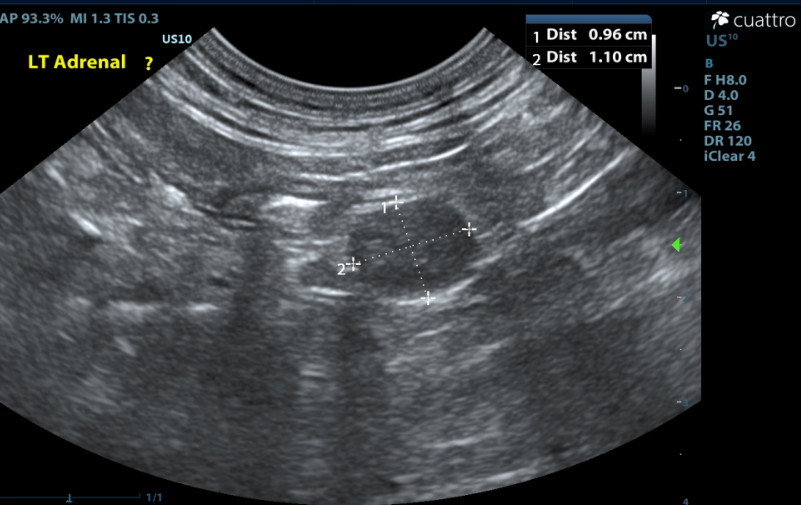
Adrenal Glands --Both adrenal glands were visualized and recognized as having normal position and echogenicity for this breed. The left adrenal is moderately enlarged and rounded in shape, measuring 10.0mm x 11.0mm. The right adrenal is mildly enlarged, but of normal shape, measuring 6.5mm in depth. No adrenal invasion into the vena cava nor phrenic vein thrombosis was noted upon color doppler interrogation. No dystrophic mineralization or clinically significant nodular changes were noted.

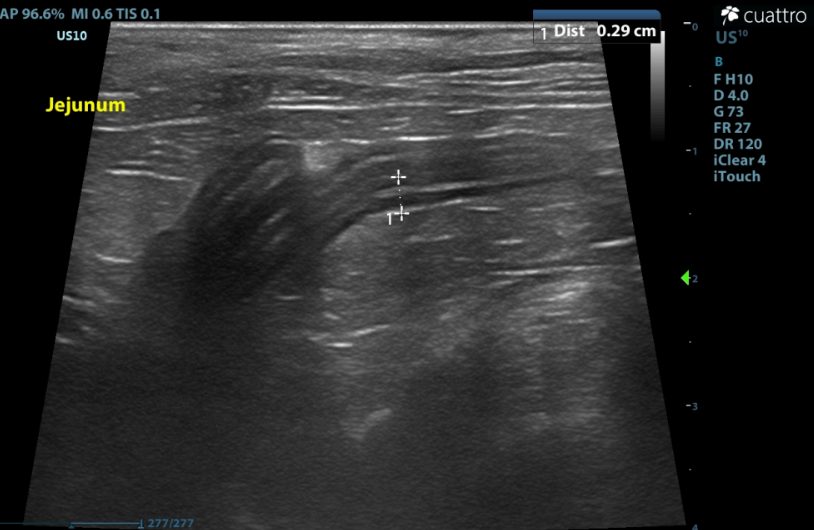
Intestinal Tract - Many to most loops of intestine are prominent to mildly thickened. Many have abnormal layering with prominent disproportionate thickening of the muscularis layer. No obstruction or masses seen.
Maximum wall thickness: Stomach-1.9 mm; Duodenum - 3.0 mm; Jejunum - 2.9 mm; Colon - 1.1 mm.
(normal wall thickness ~2.2-2.5mm, > 2.8mm abnormal Norsworthy/Estep et. al. JAVMA, Vol 243, No.10, November 15, 2013)
RECOMMENDATIONS:
London's scan revealed a moderately enlarged left adrenal and a mildly enlarged right adrenal. PDH is a possible differential, but not likely in this case, since London was hyporexic and losing weight. Chronic stress from surgery and chemotherapy was another differential to be considered, though also unlikely. London's kidneys showed moderate changes consistent with CKD. These findings, along with hypokalemia and azotemia, are consistent with CKD, but hyperaldosteronism is an additional consideration.
-Consider urinalysis with urine culture and sensitivity as well as systemic blood pressure, if not already performed.
-An aldosterone level could be submitted to rule out hyperaldosteronism. (A normal, but borderline high aldosterone level can be diagnostic in the presence of hypokalemia).
-Recommend continued monitoring renal parameters, systemic BP and electrolytes as clinically indicated. -Continue supportive care for CKD to include: fluid therapy, potassium supplementation, phosphorus binders, commercial kidney diet and appetite stimulants.
-Consider 3-view chest radiographs to further evaluate for evidence of metastatic disease (or other). -Consider endoscopic biopsies of the intestinal tract (when stable for anesthetic procedure) since disproportional thickening of the muscularis layer was observed.
-Consider diet change to novel protein diet appropriate for renal disease.
-Consider broad spectrum prophylactic deworming and fecal analysis if not already performed. -Consider a Texas A&M GI panel if not already done.
ADDITIONAL DIAGNOSTICS:
Baseline Aldosterone level- Michigan State University via Antech Diagnostics
Results= 1010 pmol/l HIGH N= 198-388 pmol/L
Systolic BP= 160 mmHg
OUTCOME:
The patient returned for a recheck exam to check systemic blood pressure. The blood pressure was only mildly elevated, but the method of measurement was not documented. The cat was prescribed Spironolactone at 2mg/kg twice daily and Potassium gluconate at 0.5 mmol/kg twice daily. A recheck chemistry panel and blood pressure was scheduled for two weeks after beginning the medications. Since both adrenals were enlarged, although asymmetrically, surgical referral for adrenalectomy was not considered at this time. The owner also declined referral due to this cat’s comorbidities. Therefore, the owner only agreed to treat medically.
DISCUSSION:
Hyperaldosteronism, also known as Conn’s syndrome, is considered the most common adrenocortical disease in cats. This is an endocrine disorder characterized by the excessive and independent secretion of aldosterone from the adrenal glands. Although, likely the most common adrenal disease in cats, it is significantly underdiagnosed because its symptoms often mimic chronic kidney disease (CKD), or in many cats CKD is preexisting.
The condition is normally classified as primary hyperaldosteronism (PHA) being caused by adrenocortical tumors. These are most frequently unilateral adenomas or adenocarcinomas, which are typically surgical. A less frequent cause is bilateral nodular hyperplasia, which is treated medically.
Clinical signs are mainly due to the severe potassium depletion and systemic hypertension. Muscle weakness is usually manifested as cervical ventroflexion, a plantigrade stance, and difficulty jumping.
Sudden blindness, dilated pupils, or hyphema can be seen due to retinal detachment or hemorrhage. Heart murmurs and arrhythmias are common. Renal symptoms, including PU/PD, are also typically present .
Since clinical signs are vague and mimic CKD, a definitive diagnosis requires specific testing. The presence of the collection of clinical signs, including hypokalemia, hypertension, plantigrade stance and adrenal enlargement or mass, give a high index of suspicion. The gold standard screening test is the Aldosterone: Renin Ratio (ARR), however, few veterinary labs are offering this testing. A fludrocortisone suppression test may be used to confirm autonomous aldosterone production, but is equally infrequent testing in veterinary labs, and can be difficult to interpret. A simple aldosterone level can be diagnostic, especially if the level is borderline to high in the face of hypokalemia.
Unilateral adrenalectomy is the treatment of choice for single adrenal tumors and can be curative. However, in animals with bilateral adrenal enlargement or patients unsuitable for surgery, medical treatment may be pursued Medical treatment includes antihypertensives, such as amlodipine and aldosterone antagonists, such as spironolactone, along with potassium supplementation.
Prognosis is excellent with successful surgery. Medical management can offer stabilization for several months to years, though kidney disease will likely continue to progress.
REFERENCES
1. Ash RA, Harvey AM, Tasker S. Primary hyperaldosteronism in the cat: a series of
13 cases. J Feline Med Surg 2005;7:173–82.
2. Chiaramonte D, Greco DS. Feline adrenal disorders. Clin Tech Small Anim Prac
2007;22:26–31.
3. Duesberg CA, Nelson RW, Feldman EC, et al. Adrenalectomy for treatment
of hyperadrenocorticism in cats: 10 cases (1988–1992). J Am Vet Med Assoc
1995;207:1066–70.
4. Javadi S, Djajadiningrat-Laanen SC, Kooistra HS, et al. Primary
hyperaldosteronism, a mediator of progressive renal disease in cats. Dom Anim
Endocrinol 2005;28:85–104.
Thanks to Dr. Allison Bodner and the staff of Sunshine Animal Hospital in Tampa, Florida

