Decembers Case of the Month - 2025
HEPATOBILIARY MASS IN A GERIATRIC CAT
Patient Information: Age: 15 years Gender: Neutered Male Breed: DSH
HISTORY: The patient presented for a non-productive cough and had a history of coughing and nasal congestion in the past. Upon presentation, it was reported that the patient had a decreased appetite as well as persistent diarrhea of a few weeks duration. No vomiting was reported and the patient’s water consumption remained normal. Physical examination revealed unintentional weight loss.
PHYSICAL EXAM FINDINGS:
Temp=101.2, P=150, R=48, wnl, BAR; Weight: 5.56lbs/2.52kgs BCS: 3.5/9; CRT/MM: <2 sec, pale,tacky; Coat/Skin: wnl, no parasites noted; Eyes: clear, wnl; Ears: clean, wnl; N/T: crusty around nose, green/brown discharge; Oral: dental calculus: 2/4, normal occlusion; H/L: grade 2/6 murmur; GI/UG: tense on palpation; M/S: loss of muscle mass; Neuro: wnl, normal mentation; PLN: wnl, symmetrical and normal consistency.
LABORATORY ABNORMALITIES:
WBC 21.97 10^9/l
Neutrophil 19.96 10^9/l
HCT 24.23%
Globulin 5.6 g/dL
Total T4 1.2 ug/dL (normal)
Liver values (ALT, ALP, GGT, Tbili) WNL
RADIOGRAPHIC FINDINGS
STUDY: Three-view whole-body radiographs
THORAX:
• The cardiac silhouette and pulmonary vessels are within normal limits.
• There is a mild diffuse broncho-interstitial pattern throughout the lungs.
• The pleural space and mediastinum are unremarkable.
ABDOMEN:
• The included portion of the abdomen is unremarkable.
MUSCULOSKELETAL: • There are chronic healed rib fractures of the left eighth, ninth, and 10th ribs.
Assessment:
1. Mild broncho-interstitial changes. Consider chronic allergic/inflammatory lower airway disease. Alternative, pulmonary fibrosis.
2. Otherwise, unremarkable thorax. No evidence of pneumonia. No evidence of pulmonary metastasis.
3. Chronic left eighth through 10th rib fractures.
ULTRASOUND FINDINGS
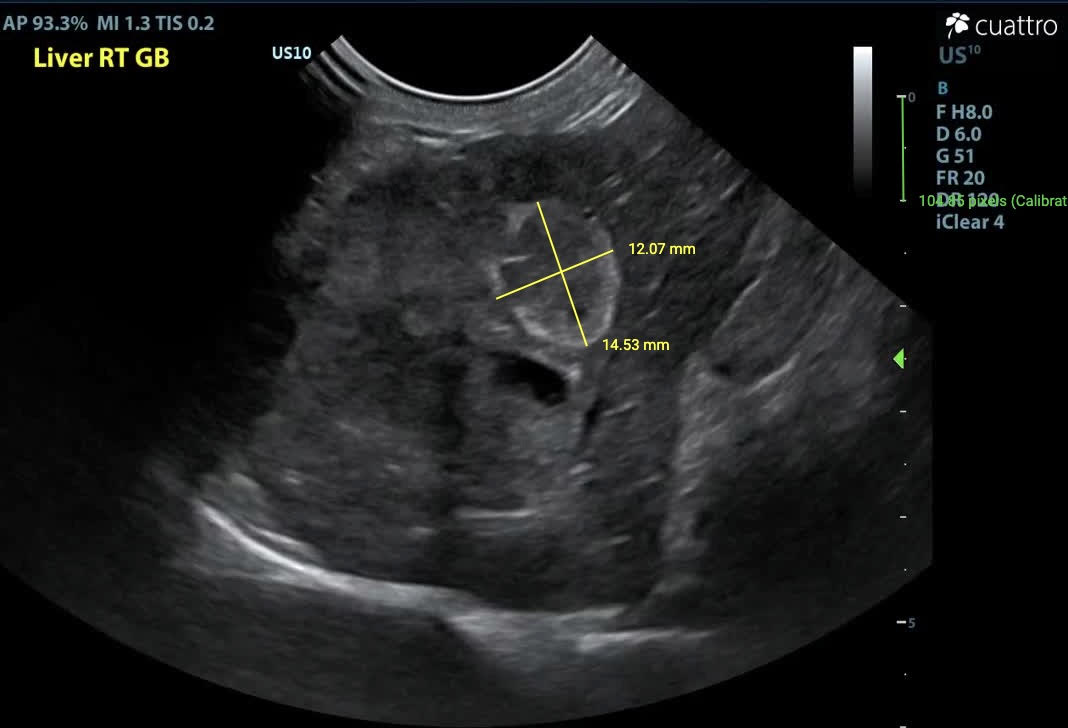
Liver - In the right liver, there is an irregularly marginated, capsule-deforming, heterogeneously hypoechoic mass measuring approximately 2.7 x 2.9 cm. Adjacent to this mass, there is an oval-shaped structure that is heterogeneously hypoechoic at the center with a hyperechoic margin, measuring approximately 1.2 x 1.5 cm. This structure may represent the gallbladder (expected) v. a second, coalescing mass. The common bile duct is dilated (5.6 mm diameter). The remaining liver parenchyma has multifocal, round, mildly capsule-deforming, hyperechoic nodules measuring up to 0.4 x 0.5 cm.
Kidneys - Normal size (Lt/Rt = 4.3/3.9 cm) and shape with coarse moderately hyperechoic renal cortices which are disproportionately large. There is mild loss of the corticomedullary junction distinction. No pyelectasia visualized.
Pancreas - Normal size (0.7 cm thickness), shape, and echogenicity. No focal lesions seen. Peripancreatic fat is normal in echogenicity. The pancreatic duct is mildly dilated (3.4 mm diameter).
Serosal Surfaces - A scant amount of anechoic free fluid is seen throughout the abdomen. No focal lesions or changes in mesenteric echogenicity noted.
Image 1: Liver mass in sagittal (between calipers) with an anechoic tubular structure extending caudally from the mass.
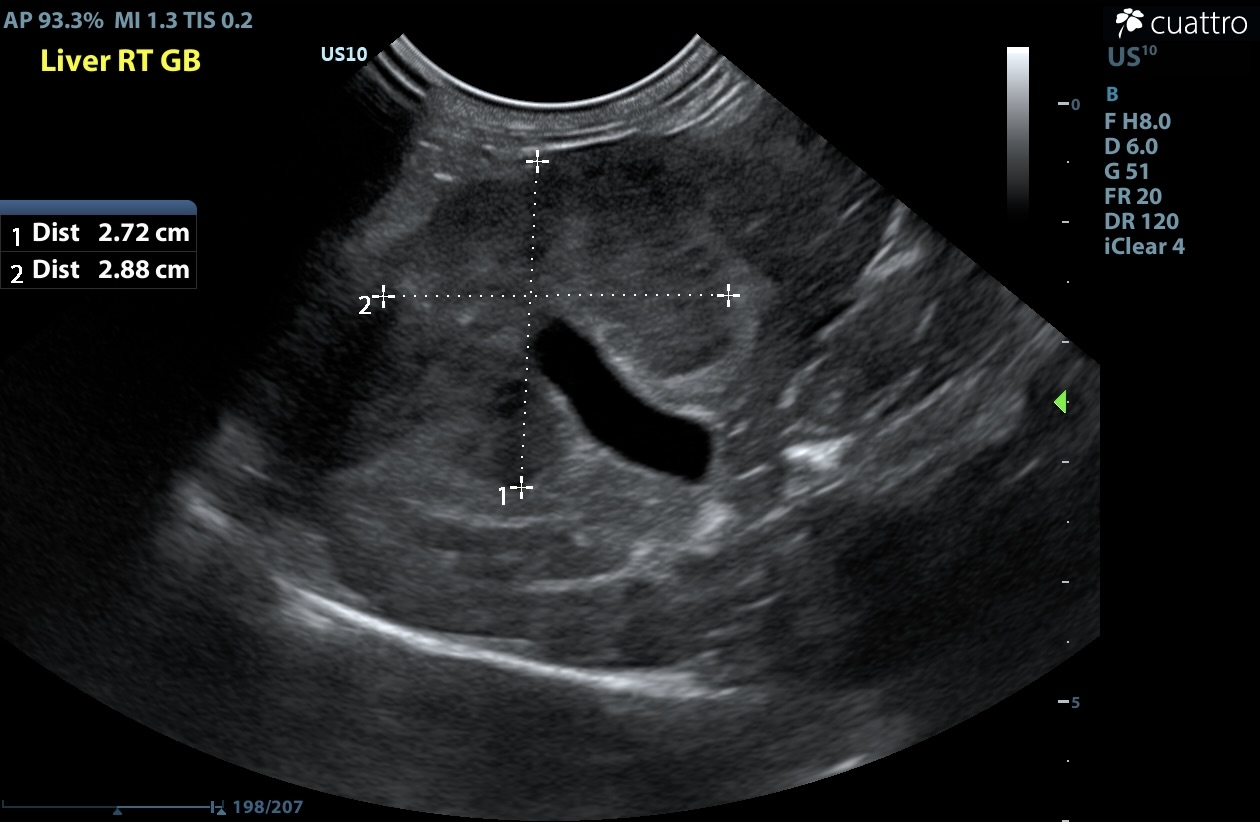
Image 2: Lack of color flow confirming the anechoic tubular structure is not vascular. This structure is the dilated common bile duct (CBD; between calipers).
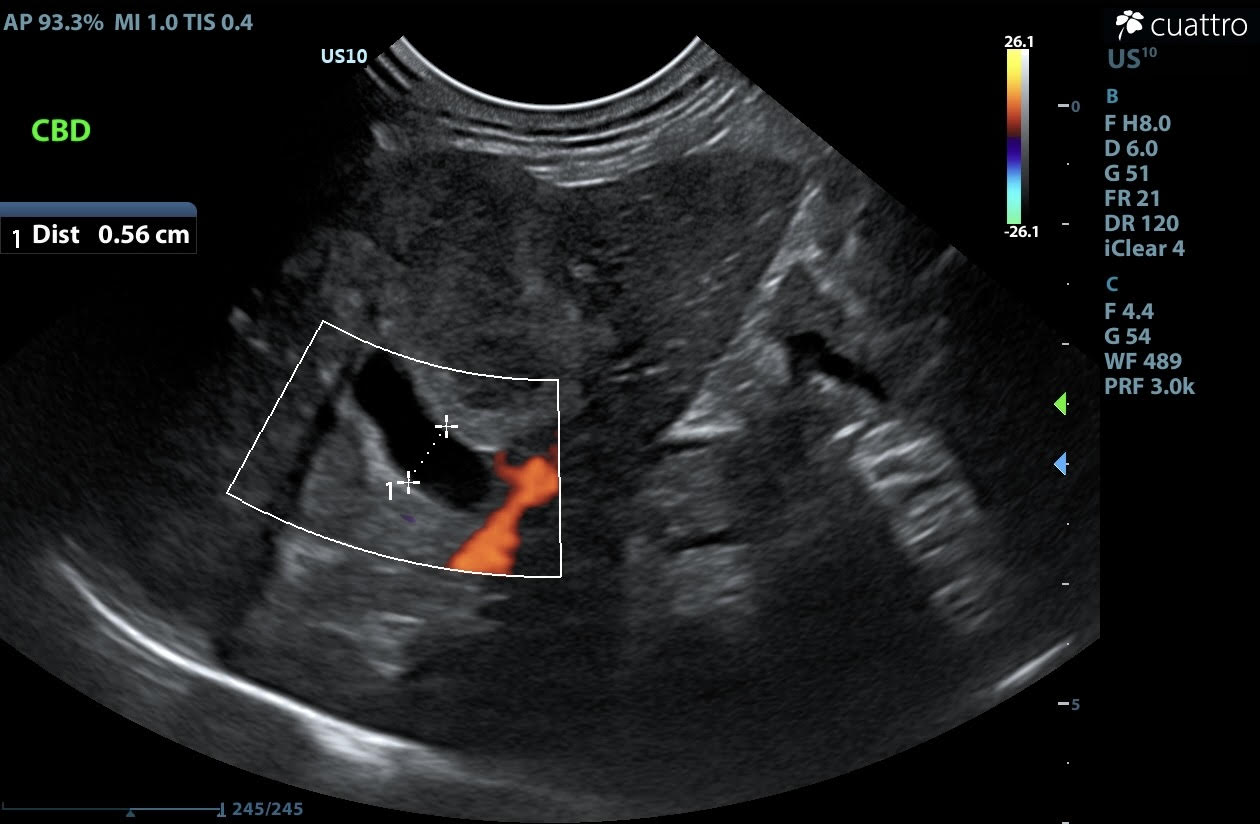
Image 3: Inflamed gallbladder v. second coalescing mass.
FURTHER INVESTIGATION:
Ultrasound guided fine needle biopsies of the right-sided liver mass were collected and submitted for cytology.
Image 4: Cytology
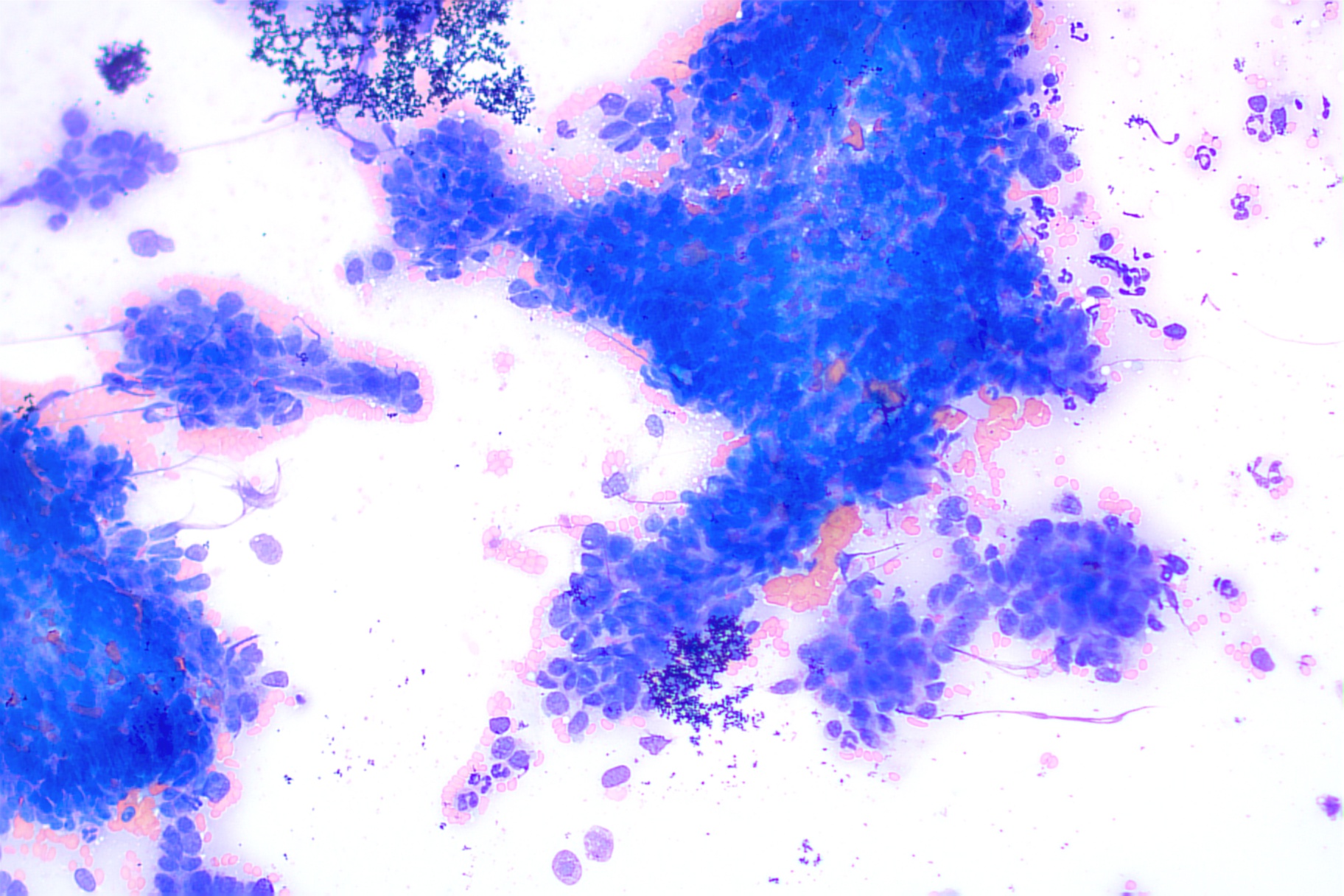
CYTOLOGIC DIAGNOSIS AND FINDINGS:
The cytologic findings are most consistent with a carcinoma at this site. Top considerations include biliary origin as well as hepatocellular origin. Biopsy with histopathology +/- immunohistochemistry would be recommended for further characterization as clinically warranted.
The sample is of focally moderate cellularity and adequate preservation. Cohesive clusters of neoplastic epithelial cells predominate in this sample with papillary-like formations, often associated with extracellular pink fibrillar material. These rounded to cuboidal cells have distinct cellular borders with a small amount of pale to medium basophilic cytoplasm. The round to oval nuclei measure approximately 1.5-3 times the diameter of erythrocyte with coarsely stippled chromatin, containing 1-2 small distinct nucleoli. Anisocytosis and anisokaryosis are moderate with a high nucleus to cytoplasm ratio. Neutrophils are rarely found on scanning, likely in accord with the degree of hemodilution. No infectious agents are identified.
DISCUSSION:
Bile duct carcinoma (BDC) is the most common malignant hepatobiliary tumor in cats, occurring intrahepatically, extrahepatically, or within the gallbladder. Prognosis is poor for cats and dogs treated with liver lobectomy, with the majority succumbing within 6 months due to local recurrence and metastatic disease. Although BDCs are histologically classified as solid or cystic, this is not prognostic, and other prognostic factors remain unidentified.
Cats with hepatobiliary neoplasia commonly present with nonspecific hematologic and biochemical abnormalities. Anemia and leukocytosis with neutrophilia may be present in up to 28% of affected cats. Generally, older animals are affected and may exhibit nonspecific, often gastrointestinal, clinical signs and increased serum liver enzyme activities. Ultrasonography can characterize hepatic lesions and guide fine needle aspiration for diagnosis.
The etiology of liver tumors is unknown, but age is considered a risk factor due to increased cell divisions and the potential for mutations. Other possible risk factors include genetics, exposure to chemicals or toxins, chronic inflammation, and hepatotoxicity. End-stage liver cancer results in hepatic dysfunction, leading to noticeable symptoms such as lethargy, diarrhea, vomiting, weight loss, jaundice, and behavioral changes; seizures may occur in severe cases. Diagnosis relies on blood work, ultrasound, and liver biopsy.
OUTCOME: The patient was provided with palliative care following diagnosis. Unfortunately, his quality of life continued to decline, and he was humanely euthanized with his primary care veterinarian.
References
Selmic, Laura E., MPH. Vet Clin Small Anim 47 (2017) 725–735. Hepatobiliary Neoplasia. http://dx.doi.org/10.1016/j.cvsm.2016.11.016
Veterinary Society of Surgical Oncology. Bile Duct Carcinoma. https://vsso.org/liver-and-biliary-tumors/#bile_duct_tumors
Carolina Veterinary Specialists. Liver Cancer in Cats - Symptoms, Treatments & Life Expectancy. https://www.huntersville.carolinavet.com/site/huntersville-veterinary-blog/2024/07/30/cat-liver-cancer
Thank you to Banfield Pet Hospital Regency and Eastern Vet Path for collaborating with us on this case.

