October 2025 Case of the Month
Patient information:
Age: 5 months
Gender: Male
Breed: Pug
Species: Canine
History:
Per the referring veterinarian, CBC - moderate nonregenrative anemia (Hct 30.6), mild leukocytosis with lymphocytosis, monocytosis, and basophilia. Chem - Elevated phosphorus (8.5), low albumin, elevations to ALT (400), alk phos (1091), and GGT (16), low cholesterol. Concern for liver shunt.
Significant Ultrasonographic Findings:
Liver:
Normal size, shape and echogenicity. No focal lesions are appreciated. The gall bladder is moderately distended with normal anechoic and hyperechoic suspended hyperechoic foci and a dependent ovoid mineralization which casts a strong distal acoustic shadow measuring approximately 0.7 x 0.3 cm that is not resulting in obstruction. No common bile duct dilation is seen.
PV:Ao = 6.7 --> A portal vein/aortic ratio of >0.8 is strongly indicative of the absence of a PSS. This value is concerning for the presence of a portosystemic shunt.
Adrenal glands:
The right adrenal gland was visualized and recognized as having normal shape, size (Rtcd - 4.6 mm), position, and echogenicity for this breed. No adrenal invasion in the vena cava, phrenic vein thrombosis, dystrophic mineralization or clinically significant nodular changes were noted.
An abnormal vascular pattern is appreciated in the left cranial abdomen which obscures visibility of the left adrenal gland.
Serosal surfaces:
Mesentery throughout the abdomen is diffusely hyperechoic.
A mild amount of anechoic free fluid is seen in several areas throughout the abdomen.
Abdominal ultrasound interpretation:
Cholelithiasis the finding is mild - DDx: Neoplasia (gall bladder, common bile duct), cholangiohepatitis, hepatitis, hypercholesterolemia, hyperbilirubinemia, hypertriglyceridemia, dietary, gallbladder dysmotility
Mesentery - the findings are mild - DDx: peritonitis - inflammation vs. paraneoplastic reaction vs. infectious vs. fibrosis vs. other.
Ascites- this finding is mild - DDx: transudate vs. hemorrhagic vs. exudate
There is a concern for a vascular shunt in this patient.
Images:
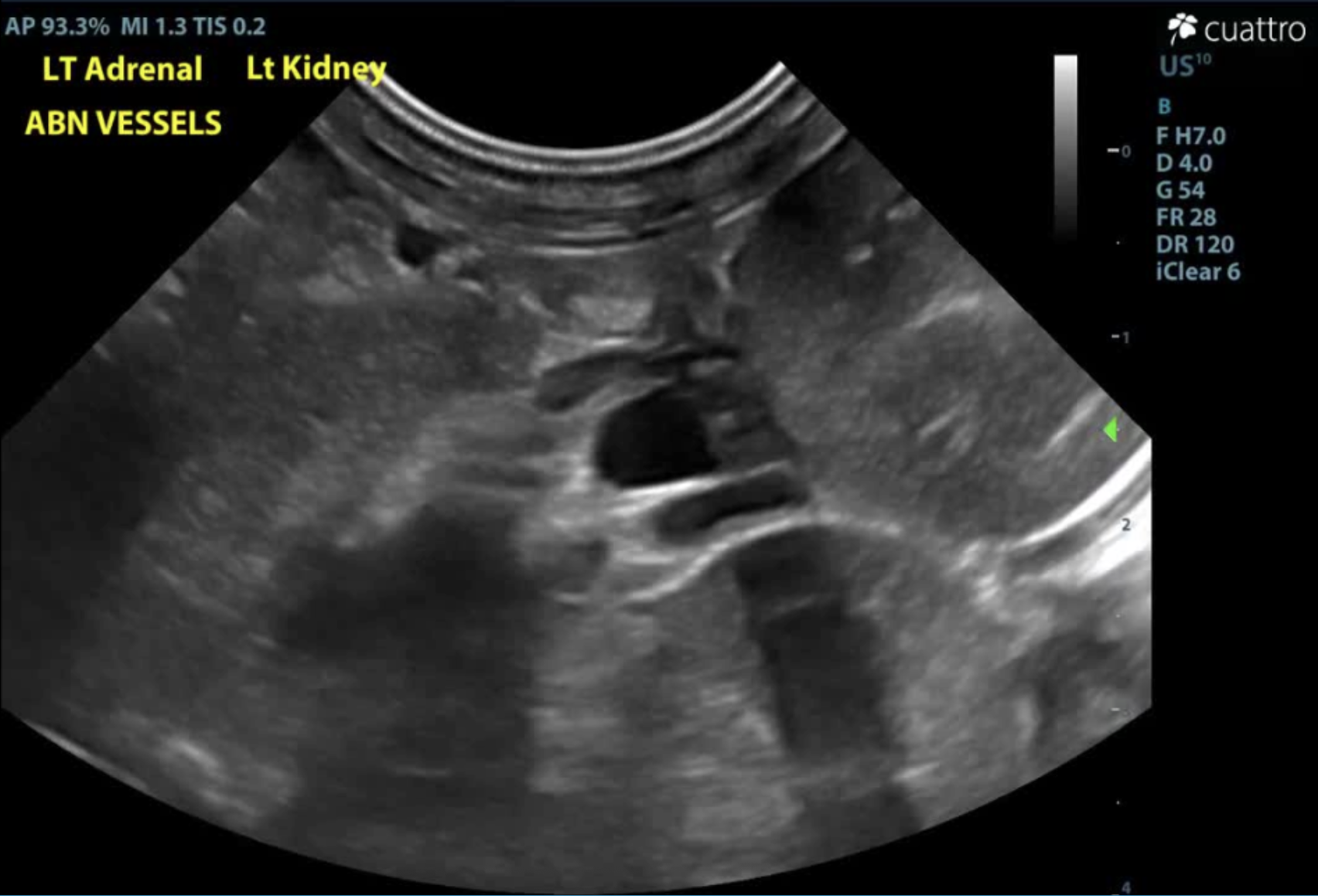

Images of irregular, tortuous vessel in the left craniolateral abdomen adjacent to the left kidney and left adrenal gland. (A) images of the vessel without Doppler coloration vs. (B) with Doppler to highlight vascular structures and the irregular pattern formation.
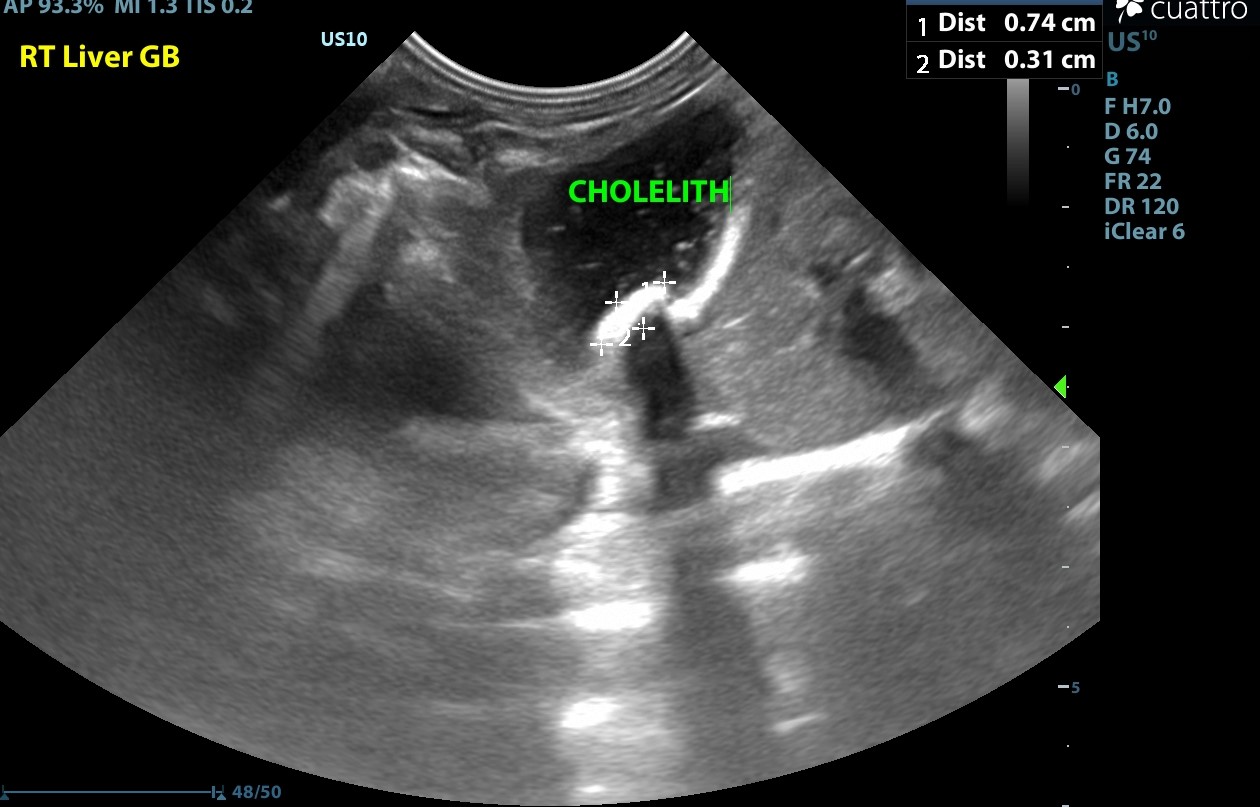
Image of organized, dependently-oriented mineralization in the gallbladder which is not obstructive. The mineralization creates a void distal to the projected ultrasound waves in a characteristic linear shape.
Recommendations:
Referral of this patient to a veterinary surgeon for advanced imaging (i.e. CT scan) and to discuss possible therapeutic options is highly recommended. While there is evidence of abnormal vascularity near the left kidney and adrenal gland, there are several parameters (microhepatica, urinary bladder stones) which do not fit the criteria for PSS. The referral recommendation is to ensure an appropriate diagnosis via advanced diagnostic imaging. Continue feeding appropriate diet which improves cognition.
Referral for CT scan (abdomen):
Study: A transverse helical multislice datasets of the abdomen was acquired. Images were reconstructed into 0.5 mm slice thickness utilizing a soft tissue algorithm. A triple phase acquisition of the abdomen during arterial, venous, and delayed phase was acquired following administration of nonionic iodinated contrast medium.
Findings: There is a large, short but tortuous vessel in the left mid-dorsal abdomen which extends from the left medial aspect of the portal vein, near the level of the renal veins and caudal to the insertion of the gastroduodenal vein into the caudal vena cava. This vessel courses leftward and dorsally and appears to insert into the caudal vena cava just cranial to the level of the left renal vein. The caudal vena cava is moderately to severely distended at this level, and the portal vein is subjectively mildly small. The mesenteric and splenic veins are also moderately generally distended. Intrahepatic portal veins are identified.
The liver is subjectively slightly small. The gallbladder contains a small amount of gravity-dependent, mineral attenuating material, and the gallbladder wall is normal in thickness. The common bile duct is severely distended (measuring up to approximately 0.8 cm in diameter). There is multifocal mineralization in one of the left intrahepatic ducts as it courses towards and inserts into the common bile duct on midline, and there is mild focal dilation of one of these intrahepatic ducts (up to 0.3 cm in diameter). No overt mineralization is seen at the level of the duodenal papilla. The spleen, adrenal glands, kidneys, urinary bladder, pancreas, gastrointestinal tract and intra-abdominal lymph nodes are normal.’
A small volume of peritoneal effusion is present.
Assessment:
- Single, large anomalous vessel consistent with a congenital extrahepatic portosystemic shunt, as described (suspected to represent a short left gastric caval variant).
- Possible mild microhepatica, secondary to the portosystemic shunt.
- Multifocal choledocholithiasis with concern for regional intrahepatic duct obstruction and obstruction of the common bile duct, given its level of
distension. The clinical significance of this finding should be correlated with the patient’s bloodwork findings.
- Mild peritoneal effusion is not considered excessive given the patient’s young age. A pathologic cause for the effusion cannot be entirely excluded.
Referral to veterinary surgeon (surgery report):
- The patient was placed in dorsal recumbency.
- Approximately 50-75 ml of clear/transparent peritoneal effusion was noted upon entry into the abdomen. The liver was subjectively smaller in size, moderately discolored (light brown with numerous yellow pinpoint foci, almost milliary in appearance) and moderately to markedly firm.
- The gallbladder was of normal color, soft, mildly to moderately dilated, but normally expressible. The cystic duct and common bile ducts were both moderately dilated without evidence of obstruction. Intrahepatic biliary ducts were not able to be visualized. - After continued exploratory, the anomalous shunting vessel was identified; it was extremely short and markedly tortuous, forming multiple acute angles on itself. The tortuous vessel was noted to originating from dorsal and deep to the stomach, coursing deep to the pancreatic and splenic vasculature, before entering the Caudal Vena Cava immediately cranial and adjacent to the left renal vein. A mild amount of turbulent flow was noted within the Caudal Vena Cava, near the point of entry of the anomalous vessel. No additional abnormalities noted during exploratory.
- Cellophane band was passed around the vessel, routinely secured with multiple alternating metallic hemoclips (3 in total). No immediate signs of intraoperative portal hypertension were noted. A guillotine biopsy was taken from the caudodorsal margin of the quadrate liver lobe.
- Patient recovered uneventfully from anesthesia.
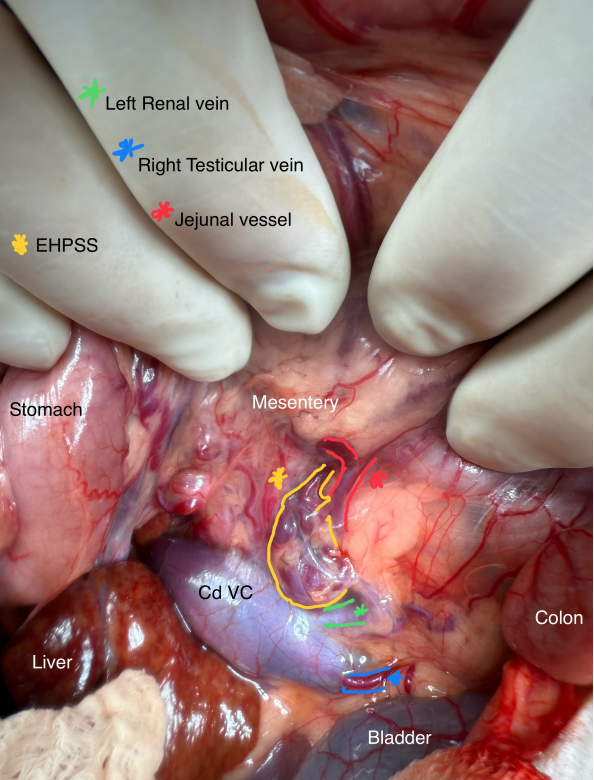
Image shows intra-operative view of intact vascular anomaly, labeled to provide a framework for the tortuous vessel. EHPSS (extra hepatic portosystemic shunt)
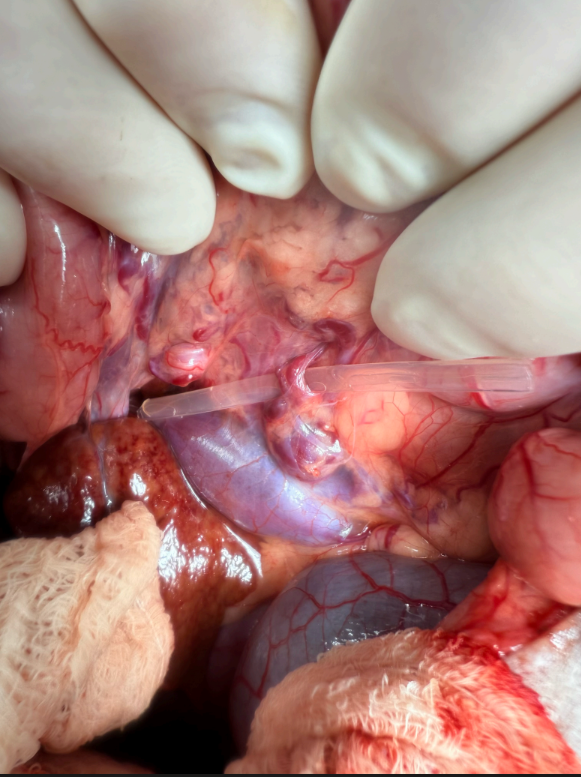
Image of the isolates shunted vessel prior to being ligated.
Histopathology:
Liver biopsy results consistent with marked, diffuse portal to portal bridging fibrosis, with marked ductular reaction. There was no evidence of neoplastic or infectious cells noted.
Discussion:
A portosystemic shunt (PSS) is an abnormal connection between the portal vascular system and systemic circulation. Blood from the abdominal organs, which should be drained by the portal vein into the liver, is instead shunted to the systemic circulation by the PSS or shunting vessel. This means that a portion of the toxins, proteins, and nutrients absorbed by the intestines bypass the liver, resulting in decreased hepatic blood flow and impairment of normal hepatic metabolic functions, and are shunted directly into the systemic circulation.
There are two categories of congenital shunts, extrahepatic (outside the liver) and intrahepatic (inside the liver). While most portosystemic shunts are congenital (the dog or cat is born with the shunt), under certain circumstances, portostystemic shunts may be acquired secondary to another problem with the liver (acquired shunts). In a normal pet, the blood that exits the intestines, spleen, and pancreas enters the portal vein, which then takes blood to be filtered by the liver. The liver metabolizes and detoxifies this blood. If a shunt is present, the liver is deprived of factors that enhance liver development (hepatotrophic factors), which results in failure of the liver to reach normal size (hepatic atrophy). A common result of hepatic atrophy is hepatic insufficiency, which then combined with the circulating toxins proteins and nutrients frequently results in hepatic encephalopathy (a clinical syndrome of altered central nervous system function due to failure of normal liver function).
The genetic basis of PSS in dogs is unknown, but it is considered congenital with breeds affected including:
- Miniature Schnauzers
- Yorkshire Terriers
- Irish Wolfhounds
- Cairn Terriers
- Maltese
- Australian Cattle Dogs
- Golden Retrievers
- Old English Sheepdogs
- Labrador Retrievers
Single extrahepatic shunts are typically congenital and more often affect small and toy breeds whereas single intrahepatic shunts more often affect large breeds. Cats nearly always have extrahepatic shunts, and the left gastric is the most common.
Acquired PSS are almost always multiple vessels, which develop in response to hepatic hypertension. They can occur in any breed or age of animal and are a compensatory mechanism to prevent or delay liver failure. As such, they cannot be ligated without causing severe symptoms, and medical management is the only option for treatment.
Patient outcome:
A 2-week post-operative recheck cleared the patient for return to full activity level due to a fully healed ventral abdominal incision.
Follow up visits with an internal medicine specialist was recommended to further discuss the liver histopathology and determine which course of therapy is best recommended.
We are grateful to Town and Country Animal Hospital and Bluepearl Veterinary Partners for their cooperation in organizing information on this story!


